Biomechanical Analysis of Gait in a Walking Boot
Introduction
Walking boots are a common form of durable medical equipment prescribed by orthopaedic surgeons for nonoperative and operatively treated injuries. However, walking boots create an iatrogenic limb length discrepancy (LLD) affects both kinetics and kinematics of gait. Altered gait leads to reported back, hip, and knee pain in patients who are prescribed walking boots.1 Currently, walking boot literature evaluates gait kinetics and ground reaction forces, focusing primarily on the lower extremities, neglecting the remainder of the kinematic chain including the spine.2–5 Our study sought to evaluate gait kinematics and kinetics in normal walking (control group), a boot group, and a boot with contralateral foot lift group (EVENup®).
Methods
Twenty participants (ages 18-40) without recent musculoskeletal trauma or pathology were included. Nineteen participants’ data were analyzed. Reflective markers were placed on the appendicular and axial skeletons. Three walking conditions (normal walking, boot and shoe, boot with contralateral foot lift (CFL)) and two speeds (2.5 mph, 3.5 mph) were randomized. Data were captured at 200 Hz (marker position) and 1200 Hz (ground reaction forces) using Cortex software and analyzed with Visual 3D and Statistical Parametric Mapping (SPM) with MATLAB. Joint moments were calculated via inverse dynamics. A two-way repeated measures ANOVA evaluated the effects of the CAM boot with/without CFL.
Results
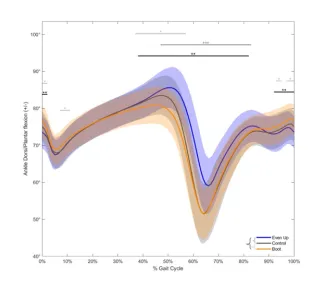
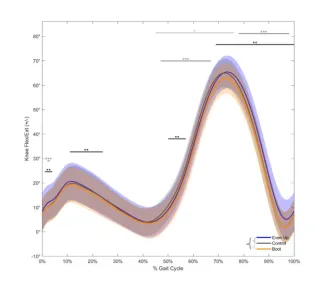
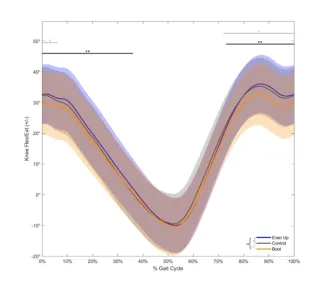
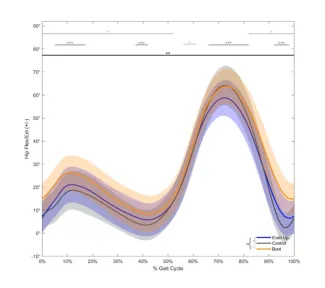
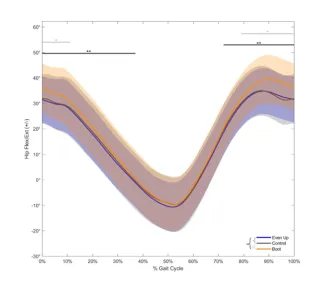
- Boot Effects: The boot decreased contralateral ankle dorsiflexion by 2.43° ± 0.87° and knee flexion by 2.90° ± 0.79° (terminal stance/swing), and hip flexion by 2.70° ± 0.26° (swing). The boot increased boot limb knee flexion by 5.94° +/- 1.84 (stance), 10.41 +/- 3.59° (swing), hip flexion 3.34°+/- 0.52 (heel strike) and 4.45°+/- 1.63 (swing)
- CFL Effects: CFL normalized CL ankle movement in stance phase, increased dorsiflexion 5.45° ± 3.44° (swing), increased CL knee flexion (3.75° ± 0.82°), and normalized bilateral hip flexion compared to controls. In the boot limb, CFL slightly increased knee flexion during stance but decreased 4.71° ± 0.71° (swing) compared controls and decreased 5.00+/- 2.39° compared to the boot-only group (100% gait cycle)
- Pelvic and Spinal Movements: Pelvic obliquity increased 1.51° ± 0.28° (swing) with CFL and decreased 1.10 +/- 0.23° (stance) in boot group. Truncal forward flexion increased 1.76° (0-24%) and 2.54 +/- 0.24° (29-100%) compared to controls. Truncal lean towards boot limb decreased 1.31° (100%); Truncal rotation towards the boot limb decreased by 1.37+/- 0.18° (preswing/initial swing). No significant changes were observed in pelvic tilt.
- Kinetics: CFL decreased joint moments on the BL ankle, normalized knee flexion moments, decreased knee adduction and rotational moments, and decreased hip abduction and rotation moments with minimal changes to sagittal plane moments. CFL normalized CL ankle sagittal plane moments, decreased CL ankle adduction moments (stance), decreased CL knee flexion, adduction, and rotation moments (stance) compared to controls, and increased hip extension moments (stance) in both CFL/boot groups while decreasing hip abduction moments in CFL group.
Tables and Figures
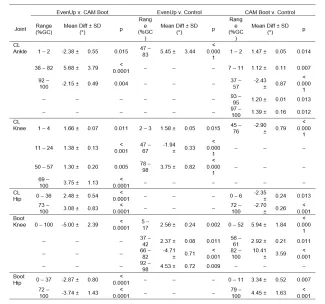
Table 1
Results of the t-test posthoc analyses for the five reported joint kinematics (contralateral (CL) ankle, knee, and hip, and the Boot knee and hip). Mean difference is reported as the difference from the control. For the hip and knee, flexion/extension (+/−) is reported and for the ankle, dorsi/plantar flexion (+/−).
Figure 1
Sagittal ankle angle of the contralateral limb. Significance bars using *, **, and *** indicate significant differences between the EvenUp v. Control, CAM Boot v. Control, and EvenUp v. CAM Boot conditions, respectively.
Figure 2
Sagittal knee angle of the contralateral limb. Significance bars using *, **, and *** indicate significant differences between the EvenUp v. Control, CAM Boot v. Control, and EvenUp v. CAM Boot conditions, respectively.
Figure 3
Sagittal hip angle of the contralateral limb. Significance bars using *, **, and *** indicate significant differences between the EvenUp v. Control, CAM Boot v. Control, and EvenUp v. CAM Boot conditions, respectively.
Figure 4
Sagittal knee angle of the limb with the Boot. Significance bars using *, **, and *** indicate significant differences between the EvenUp v. Control, CAM Boot v. Control, and EvenUp v. CAM Boot conditions, respectively.
Figure 5
Sagittal Hip angle of the limb with the Boot. Significance bars using *, **, and *** indicate significant differences between the EvenUp v. Control, CAM Boot v. Control, and EvenUp v. CAM Boot conditions, respectively.
Discussion
A walking boot alters gait kinematics, particularly increasing knee and hip flexion in the BL while decreasing CL flexion to accommodate for the acquired LLD. Addition of a CFL normalized BL knee flexion during stance phase, decreased knee flexion during swing phase, and normalized bilateral hip flexion angles compared to controls. Interestingly, minimal angular differences were observed in pelvic and spinal kinematics between either intervention, but more symmetrical gait was observed in the CFL group, which could alleviate secondary site lumbar back pain experienced with walking boots. Overall, joint moments were improved in the CFL group except for CL hip extension moments which increased in both groups. This corroborates previous reports indicating the CL hip as the second most common secondary site of pain in a walking boot.1 We suspect limited pelvic and spinal parameter changes are likely a result of young, healthy participants. Older populations may not be able to compensate for LLD resulting in more drastic changes in spinal alignment.
Conclusion
Our findings support the use of a CFL with a walking boot to reduce joint motion and moments on the injured limb, promoting better gait symmetry in the lower extremities with minimal differences in the pelvis and spine. Further studies in older populations may reveal more significant changes in axial alignment.